Prior authorization can take time to process, and it depends on what procedure your physician is prescribing and the insurance company agreeing to cover any part of the costs. If these can’t be agreed upon, you can ask your physician if he or she will provide a generic instead of the name brand, or find another health plan that covers name-brand prescriptions. Within a week of submitting a prior authorization to your pharmacy, you should receive notice one way or another as to whether your prescription was approved.
Advocate for your Care
Prior authorization means that your physician must follow a process to obtain prior approval from your insurance company when administering specific medications, medical devices, and medical procedures. The insurance company or plan will provide full or partial coverage. Sometimes, the insurance company denies a physician’s request.
There are several ways to ensure your doctor will obtain prior authorization from your insurance company. Having a conversation with your insurance provider is one way you could check. If your doctor has not filled out any prior authorization requests, you can check in person at the pharmacy.
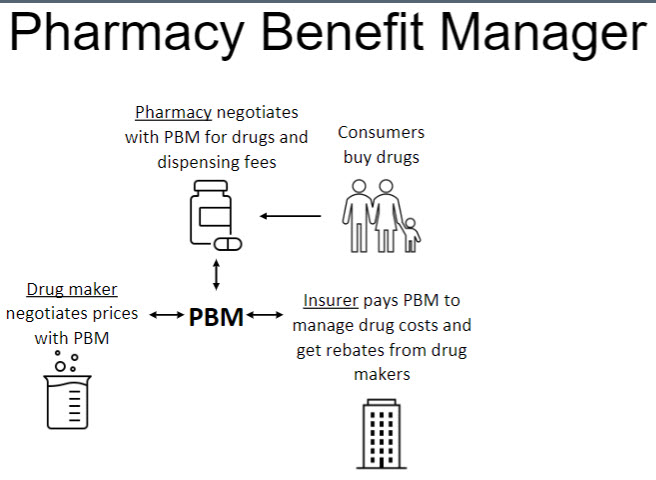
LPBM – Pharmacy Benefits Managers
Pharmacy benefit managers are an essential component of the pharmaceutical industry. They develop formularies, negotiate lower prices with drug manufacturers, and control drug spending to name-brand effective drugs for consumers. Because of this, it is vital for healthcare managers in clinics to be aware of PBM studies as they are released, which provide up-to-date information regarding pricing information for drug makers and insurance companies or pharmacies from which consumers buy their drugs. This information is necessary for a well-rounded modern clinic; those unable to keep pace with PBM studies will suffer from inaccurate information, creating confusion among workers and patients. (Johnson & Walston, 2020, p.93)
https://online.vitalsource.com/books/9781640551466
Conclusion
To get a prescription filled, you usually have to get approval from your insurance company. If it’s a name brand medication, you also need approval from your health plan. And if it’s a new drug, or a generic version of a prescription you already take, then you may need approval from both insurers and the pharmacy’s
benefits manager.
If you need prior authorization or want to know why a prescription was denied, you can contact your insurance plan or visit www.healthcare.gov/prior-authorization. You can also visit our other post of Prior-Authorizations.
Reference