With the growing complexities of healthcare, Prior Authorization (PA) has emerged as a crucial player in healthcare delivery. As a preventive measure implemented by insurance companies, PA requires physicians to request approval before offering specific services or drugs to patients. Here, we shall delve into some critical statistics around PA, its approval rates, appeals, and timeline.
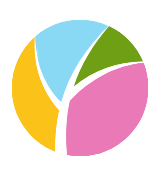
Physicians’ encounters with PA demonstrate an impressive approval rate – 72% of PA requests are approved initially, and an additional 7% are permitted on appeal. These figures suggest a largely efficient process; nevertheless, there’s more to consider beneath these surface-level numbers.
PAs: A Timed Affair
One key element in understanding PA is appreciating its time-bound nature. PAs are granted for a specified duration, post which physicians must resubmit requests for continued prescription refills or therapies. This recurrent procedural necessity does add substantial administrative work for healthcare providers and may potentially impact the efficacy of care delivery.
Unpacking the Timeline
When focusing on timelines, 2018 data reveals that response times for PA requests were reasonably adequate. Nearly half (48%) of all PA requests received a response within one business day. A further 19% received a response within two days, while approximately 26% waited three business days or longer. Interestingly, 7% of physicians were unsure about average wait times – highlighting a potential need for greater process transparency from the insurance companies. (Center for Value in Health Care, Altarum)
Denial is not the End
Admittedly, not all PA requests are approved. The data indicates an approximately 6% initial denial rate. However, a denial is far from the final word as an appeals process exists and is successfully leveraged quite regularly, particularly compelling is the appeal success rate. Of the initially denied requests, 11% appealed, with an overwhelming 82% of these appeals resulting in a full or partial overturning of the initial denial.
Variables at Play
While these numbers offer considerable insight, they aren’t static and can fluctuate based on several factors. The type of healthcare service requested, the specific healthcare provider, and the patient’s health insurance plan are but a few of the many variables that can swing PA approval rates or timelines.
According to KFF using data from 2021 that note, 11% of prior authorization denials are appealed. Yet, a strong 82% of these appeals result in a fully or partially overturned initial denial. This paradox underpinning appeals reinforces the importance of understanding and leveraging the intrinsic appeals process within PA protocol.
Carefully optimized navigation through the maze of PA, along with a clear understanding of existing benchmarks and key variables, is sure to help healthcare providers in backing best practices for their patients.
This look at the PA process is based on insightful research by the Kaiser Family Foundation (KFF) and Altarum. Mystaffology has published additional articles on Prior Authorizations. Follow this link to read more. Their dedication to providing transparent and thorough healthcare-related insights forms the backbone of many informed decisions in healthcare today.
Sources: