Introduction
The healthcare industry is moving towards a new era, where technology and data are driving changes in how health systems operate. Just as the technology we use has changed over time, so have our healthcare designs and strategies.
Healthcare systems are complex
There are some key design choices that determine how they’ll impact patients and payers. Healthcare systems can be categorized by their structure, such as whether they’re public or private; by who has control over them (e.g., government vs. insurance companies); and by their financing method (e.g., tax-based vs. fee-for-service).
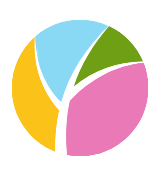
There are four main types of healthcare systems:
- Publicly funded but privately delivered–In this type of system, patients have access to both public and private providers; however, most care is provided through private providers who bill the government for reimbursement under one form or another (e.g., insurance companies). Examples include France and Germany. Governmentally controlled–In these types of systems, governments establish strict regulations on what treatments can be covered as well as pricing tiers within which doctors must operate. Voluntary/semi-voluntary–These arrangements allow people who opt into them greater freedom over which doctors they see but still require them to pay premiums each year based on income level.
Here is a quick overview of four common types of healthcare system designs:
The Beveridge model
The Beveridge model is a national health insurance model that covers everyone, regardless of age or income. The government provides coverage and pays the costs of healthcare. The government sets prices for services and drugs by negotiating with providers on behalf of individuals who are covered under this system.
As you can imagine, this type of system has pros and cons:
- Pro: Under this model, everyone has access to healthcare because it’s provided by the government (or single payer). There’s no need for people to go without needed care because they can’t afford it; instead, someone else will cover their expenses so they can get treated when needed.
- Cons: It could be difficult to control spending since there isn’t any competition between insurers trying not just provide good service but also lower costs
The Bismarck model
The Bismarck model is a type of healthcare system that provides universal coverage, including inpatient, outpatient and long-term care. Coverage is financed through social insurance, which means that all citizens are automatically covered. Private insurance companies provide the coverage at the point of service.
The Bismarck model was named for Otto von Bismarck, who first introduced this type of system in Germany during the 1880s to deliver health benefits without spending public funds or raising taxes on workers’ wages. The model has been adopted by other countries around the world, including Australia and New Zealand; however, it’s most commonly used in Europe today — particularly those nations with socialized medicine like Britain’s National Health Service (NHS).
The national health insurance model
In this model, the government pays for all healthcare costs. The government provides services to its citizens through public hospitals and clinics and often makes them available at a low cost or no cost to those who cannot afford to pay.
In this system, there is only one payer: the government. This means that all providers submit claims directly to Medicare or Medicaid (the national insurance programs) rather than filing them through their own insurance company as they would in other systems. This means that there is no competition among insurers; they don’t compete based on price but instead focus on quality standards so patients can choose which insurer best meets their needs.
Prices are set by governments rather than being negotiated between doctors’ offices and insurers like in other models discussed here today–it’s difficult for consumers to compare costs between providers or even within each type of care delivery organization itself!
The out-of-pocket model
The out-of-pocket model is the most common healthcare system in the world. In this model, people pay for their own healthcare costs directly rather than through insurance. This means that if you need medical treatment or prescription drugs, you’ll pay for them yourself instead of having an insurance company or government agency cover part of your expenses.
The out-of-pocket model has some benefits: It encourages people to be more careful about how much they spend on health care because they have to pay out of pocket; it allows them to shop around for good deals on medical services; and it provides more incentive for doctors and hospitals to provide high quality care at lower prices since patients will choose providers based on price alone if no other factors matter (e.g., reputation). This type of system also has some drawbacks: Without any limits on what insurers can charge customers who use their coverage frequently — such as annual caps — premiums could skyrocket over time due solely to inflationary pressures rather than increased utilization rates among policy holders.
Conclusion
The
healthcare system design you choose should be based on what works best for your facility and patient population. While there are many options available, some may not be a good fit for everyone. It’s important to consider all factors when choosing which type of system would work best for your hospital, clinic setting or region your facility operates. To learn more, visit our website:
www.mystaffology.com or visit
GoodRx, they have an excellent summary of the differences between the models as well.